No commercial device has successfully measured real-time vasoconstriction from the chest
If done in real time, detecting vasoconstriction could be used for several medical purposes: to assess the effectiveness and adjust the dosage of blood pressure medication, detect the potential for serious health conditions before they occur (e.g., a sickle cell attack), identify long-term trends in sympathetic neural activity and patient stress, and better understand an individual’s response to hormonal medication.
One technique currently used for vasoconstriction detection is photoplethysmography (PPG), which measures the pulsatile blood flow in an artery using an optical sensor. However, because of venous pooling, vasoconstriction manifests weakly in traditional PPG measurement locations, such as the finger, toe, and ear.
The optimal location for vasoconstriction detection is mid-sternum, but it is challenging because each patient’s chest morphology is unique and the location has poor perfusion, resulting in lower signal amplitude. Thus, no commercial device exists that has overcome these challenges to successfully measure vasoconstriction from the chest.
Flexible patch conforms to skin and mitigates motion artifacts to enable continuous PPG monitoring from the chest
This wireless, soft sternal patch includes integrated skin-like photolithographically patterned electronics that are specifically tuned to continuously measure vasoconstriction from the sternum. A biocompatible tape adheres the patch to the skin in a minimally intrusive manner, producing highly conformal skin-device contact. A pressure application and elastomer-dampening system mitigates motion artifacts in the PPG signal caused when the skin bends, stretches, or otherwise undergoes movement. Tests have shown the device is highly capable of detecting vasoconstriction that is induced endogenously through controlled breathing exercises and exogenously through changes in ambient temperature.
In overnight trials with sleep apnea patients, the device detected apnea and hypopnea with 95% precision and 100% sensitivity compared to data professionally scored by licensed clinicians. In addition to accurately detecting apneas, this device provides clinicians with critical insights into how each apnea affects the patient’s cardiac mechanics, blood oxygenation, and sleep quality.
This technology offers a new paradigm of continuous vasoconstriction monitoring. It opens the door to monitoring bio-signals from other non-traditional anatomical regions as well as integration with electrocardiography and seismocardiography sensors, which could play a crucial role in monitoring cardiac disease.
- Improve health diagnoses: As mid-sternum is the optimal location for vasoconstriction detection, attaching this patch to the chest can potentially lead to improvements in detecting key markers of numerous harmful health conditions.
- Reduce side effects: The patch can be used to identify the degree of vasoconstriction induced by medications to enable precise dosing, potentially avoiding the risk of serious side effects.
- Improve understanding of outcomes: Continuous monitoring and wireless communication enables tracking physiological outcomes (e.g., medications, dosages, and other health implications) over time.
- Broadens PPG potential: This technology has the potential to enable PPG recording in a wide range of traditionally inaccessible anatomical regions.
- Platform for multifaceted monitoring: Placing the patch on the patient’s chest enables simple integration of electrocardiography and seismocardiography sensors to create a single, all-in-one device that is capable of multifaceted human health monitoring.
This new method for continuously detecting vasoconstrictions in real time via chest-based PPG monitoring has broad and significant medical applications, such as:
- Assessing the effectiveness and adjusting the dosage of blood pressure medication
- Detecting potential for serious health events, such as a sickle cell attack, before they occur
- Identifying long-term trends in sympathetic neural activity and patient stress
- Understanding an individual’s unique response to hormonal medications
- Monitoring sleep apnea and other sleep disorders
- Monitoring shock victims
- Assessing contraction of blood vessels (e.g., replacing or augmenting expensive low-throughput MRI and CT scans by performing initial screening)
- Enabling PPG recording in a wider range of anatomical regions
Illustration of the soft sternal patch that can interact with an external device for wireless data recording.
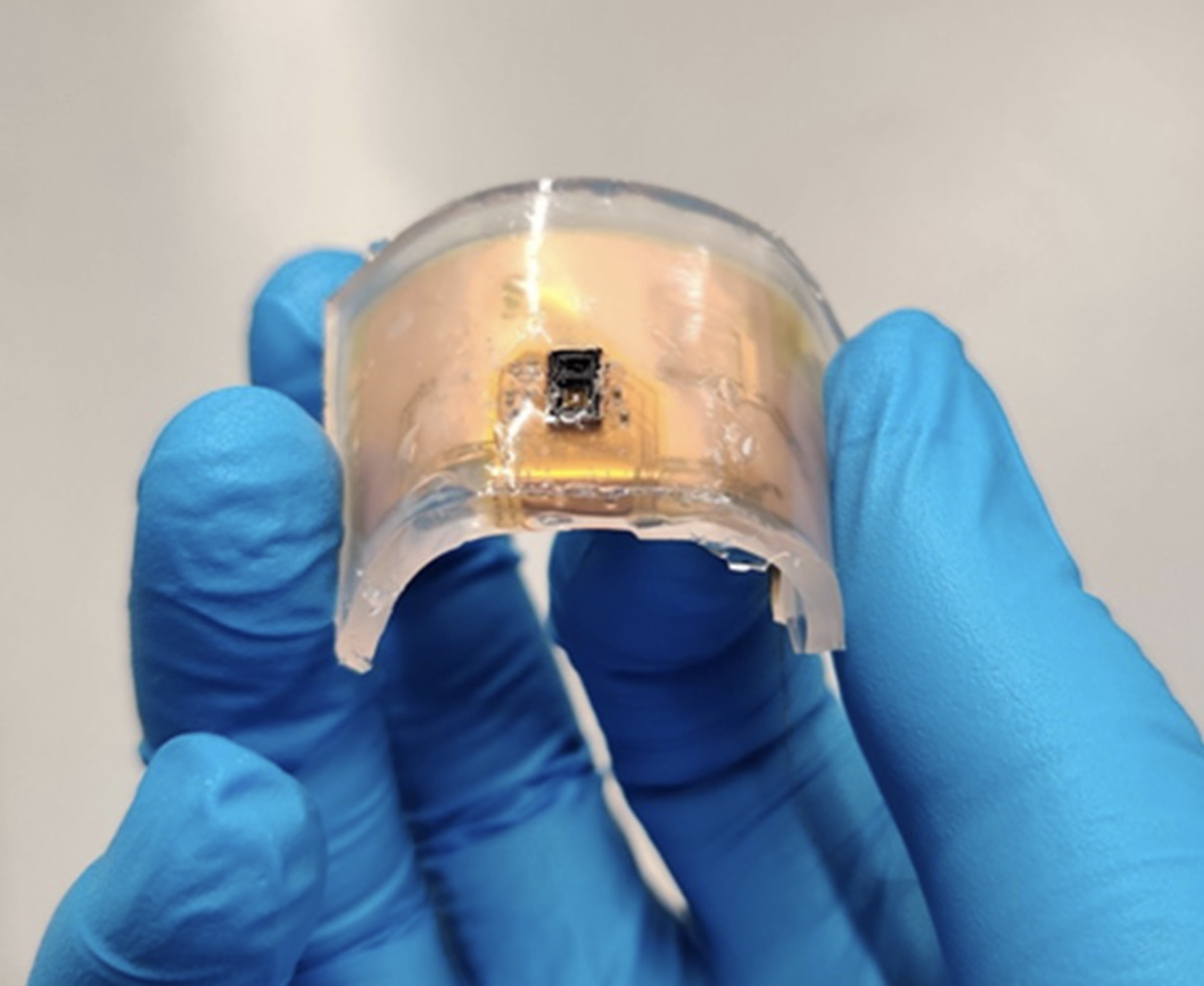
The soft patch showing flexibility.
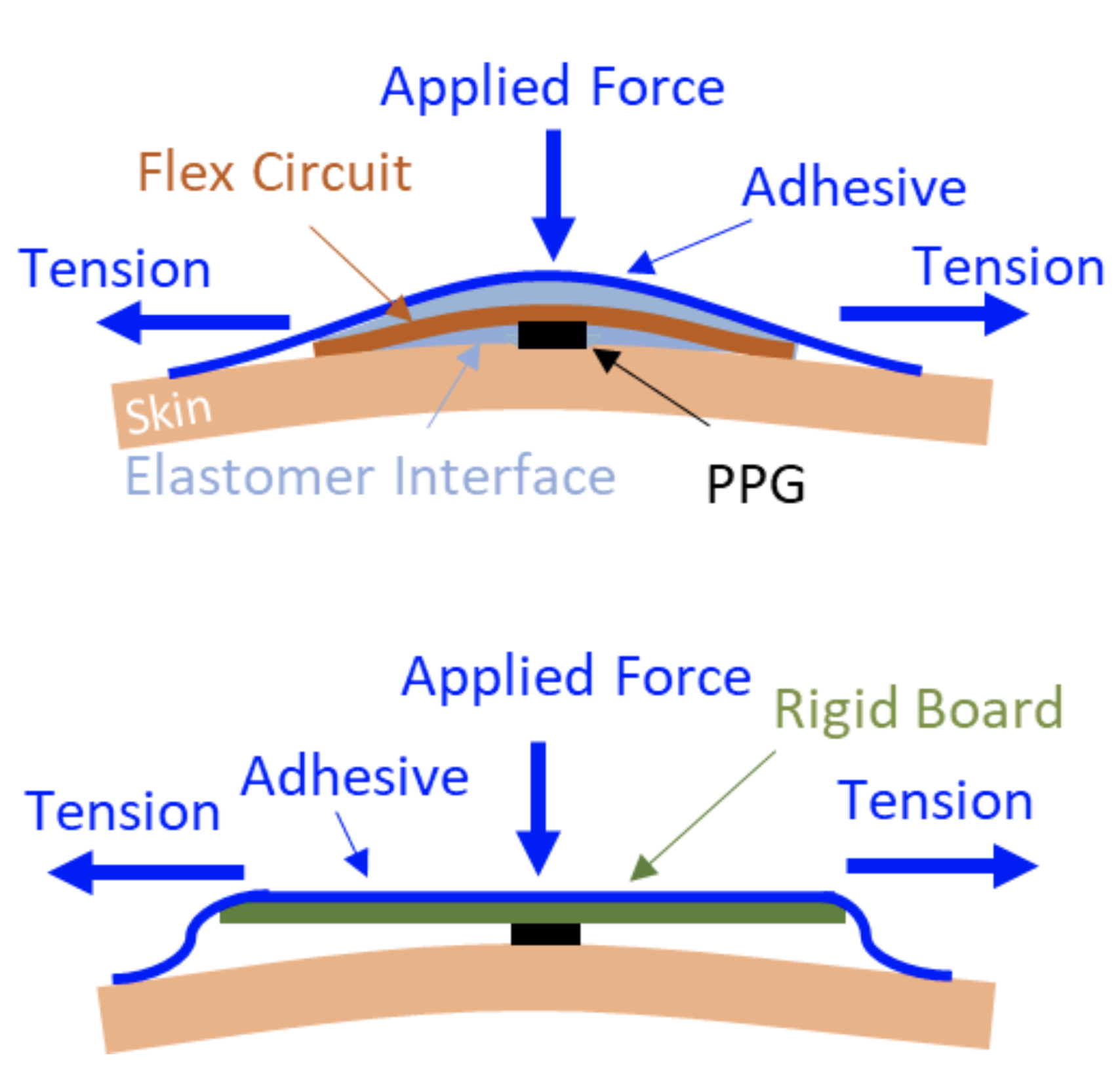
Illustrations showing a soft device’s skin-contact quality (upper) compared to a rigid device case (lower) that cannot adhere to the skin and is susceptible to rocking and translational motion artifacts.
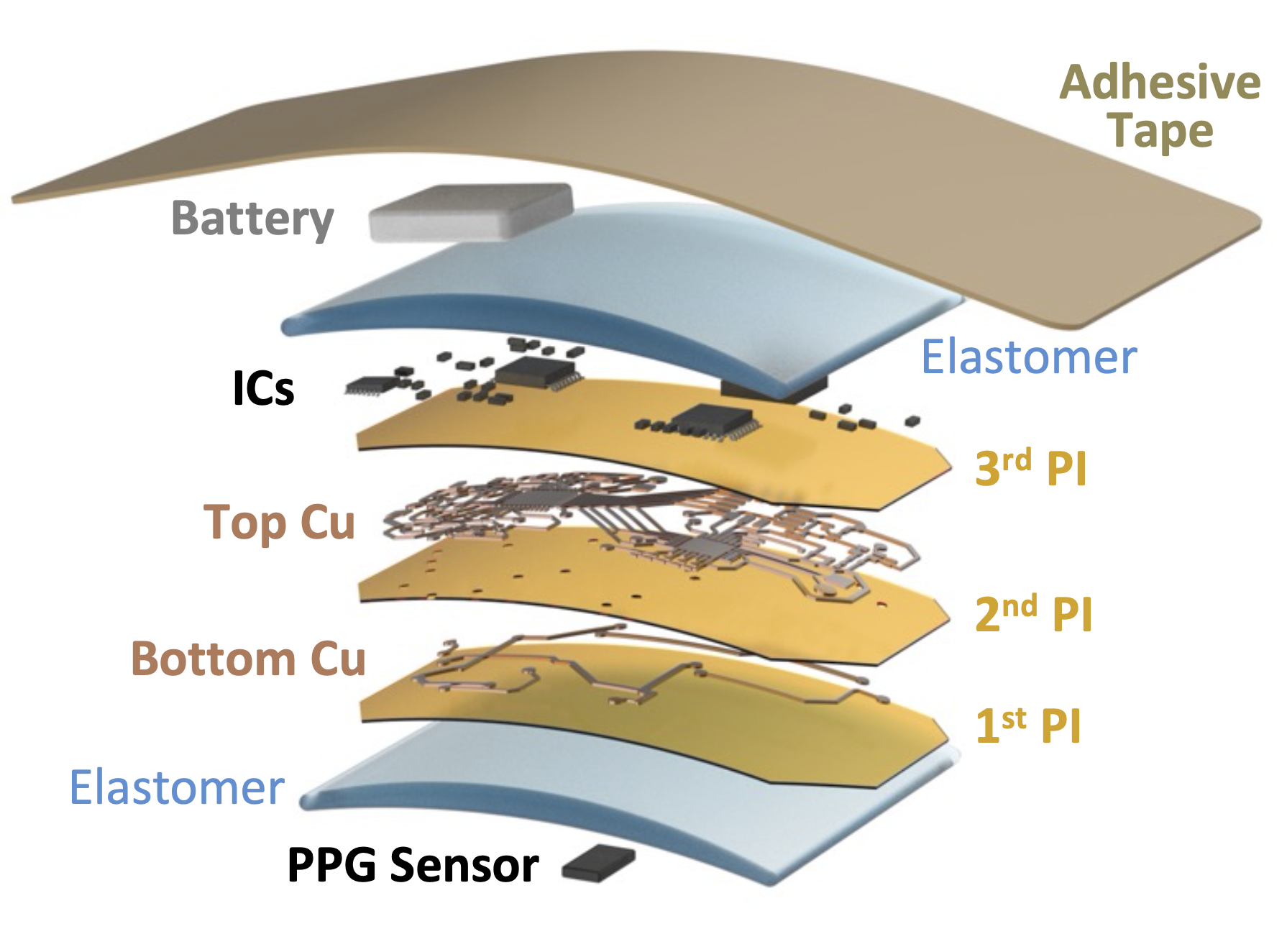
The components of the soft sternal patch include the multiple layers of the sensor, polymers, metals, electronic chips, and a battery under a soft adhesive tape.
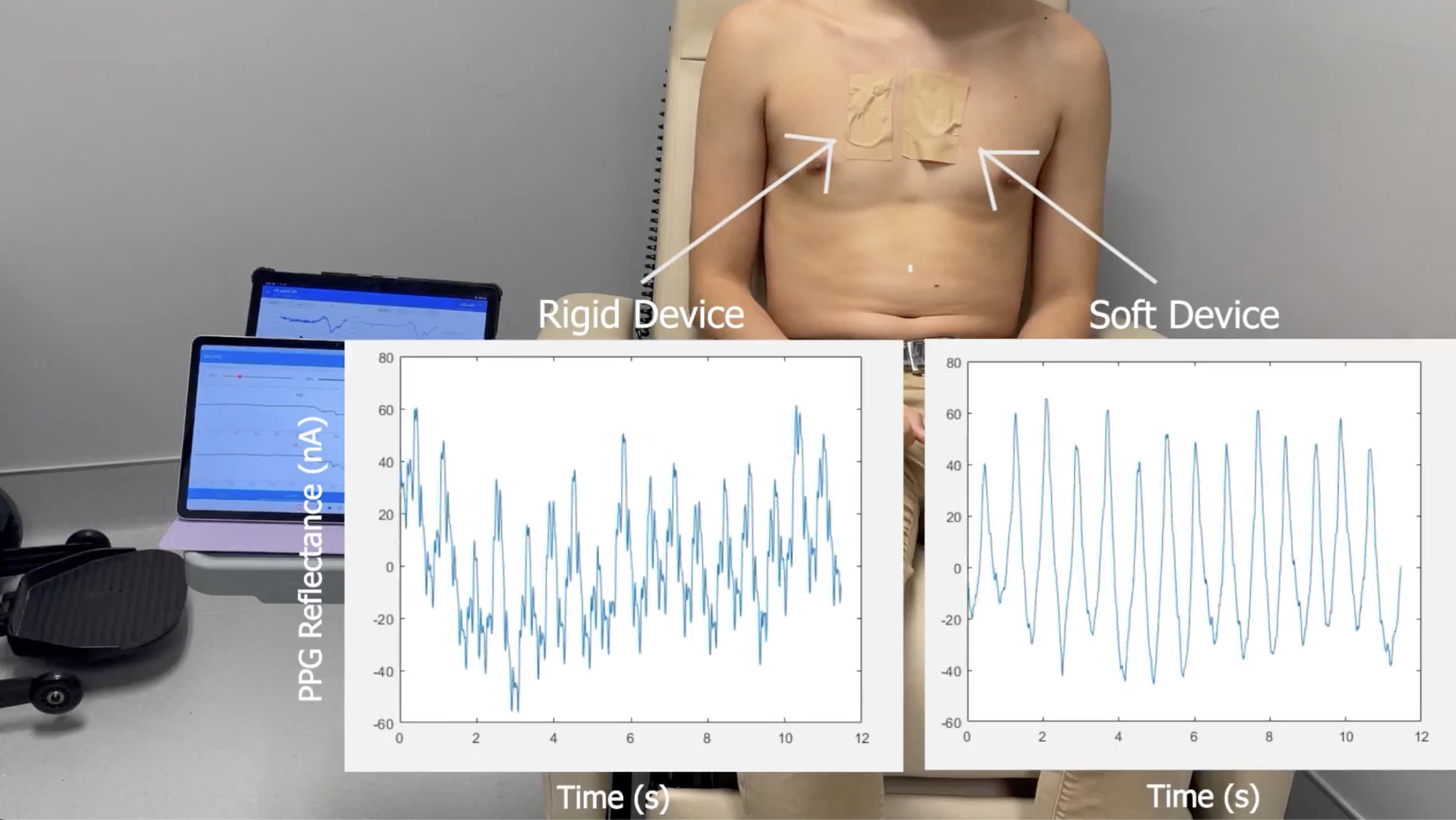
In this video, signals were simultaneously recorded in both a soft device and a rigid alternative device with identical components and footprint during skin perturbations. This video clearly shows that the magnitude and duration of motion artifacts are increased in the rigid device compared to the soft device. (https://youtu.be/qgCEyEwzZ3A)
