This non-invasive device aims to treat acute respiratory distress syndrome (ARDS) caused by COVID-19 and other viral and bacterial infections. The vest-shaped device applies localized pressure to the chest and back to simulate proning. It was designed to provide an alternative to proning, which involves positioning the patient facedown to redistribute blood to uninflamed regions of the lungs that can still participate in taking up oxygen. Georgia Tech’s device has the potential to reduce adverse events that occur due to the physical stress on patients of proning as well as eliminate hours of clinical staff effort required for the maneuver. Designed to be used in combination with mechanical ventilation, the vest might also be used for standalone oxygenation support.
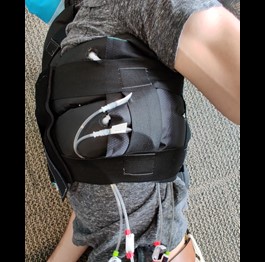
Containing independently inflatable chambers, the vest is designed to enable physicians to fine-tune and customize for each patient the redirection of blood to specifically selected locations. An electro-pneumatic system, which is operated via a graphical user interface, autonomously controls the pressure of each chamber, depending on patient needs. Each compartment can be inflated up to 6 psi gauge pressure with precision of 0.1 psi.
Currently, a single vest can accommodate patients with chest circumferences from 35 inches to 60 inches. Constructed from soft thermoplastic polyurethane (TPU)-backed nylon fabric and TPU film, the vest consists of three separate pieces that are heat-welded together to simplify the donning process.
- Powerful: Designed to optimize oxygenation for patients in acute hypoxic respiratory failure
- Supportive therapy: Non-invasively complements mechanical ventilator support
- Low cost: Significantly less expensive than technologies that increase oxygenation (e.g., ventilators, oxygen systems)
- Easy to use: Reduces the need for specialized equipment, training, and facilities
- Customized: Independently inflates the various chambers, potentially allowing individual parameters to be optimized for each patient
- Treatment for ARDS resulting from COVID-19, mycoplasma pneumonia, sepsis, and other viral and bacterial infections that affect the pulmonary system
- High-frequency oscillation for pulmonary mucus expulsion (e.g., cystic fibrosis, chronic obstructive pulmonary disease (COPD))
In acute severe respiratory failure due to COVID-19, critical care recommendations include placing facedown patients who are dependent on mechanical ventilator support for their survival. This position—known as proning—physically redistributes blood to uninjured or minimally injured lung tissue and has been demonstrated to improve ventilation and perfusion for some COVID-19 patients.
However, not all critical care centers are equipped or trained for the maneuver, which is labor intensive and does not always produce desired results. Generally, five to eight hospital staff members are needed to safely prone a single patient. Conversely, this Georgia Tech innovation is designed so that just two or three staff members can place the V/Q vest on a patient, and one staffer can monitor its use.

Early prototype of Georgia Tech’s V/Q Vest designed to treat acute respiratory distress syndrome