Through the genetic reconfiguration of T-cells to include heat-responsive biocircuitry, Georgia Tech inventors have developed T-cells that are designed to serve as a precision therapeutic against cancerous cells. Leveraging the conserved heat shock response, the engineered T-cell implanted with plasmic gold nanorods (AuNRs) can be "turned-on" at specific tumor locations, decreasing off-target effects. Research showed that the remote heat shock does not impact the T-cells’ proliferation, migration, viability, and cytotoxicity, suggesting that the programmable T-cells would be able to provide a high-efficacy response to the cancerous cells.
An additional feature of this technology is that the AuNRs allow the near infrared (NIR) light to penetrate the deep tissue, which would enable the monitoring of cellular biomarkers’ activity.
- Specific: The remote programmable nature of these T-cells allows them to be selectively activated only in the necessary locations.
- Protective: This focused, genetically engineered immunotherapy is intended to protect patients from the additional harm of the off-target cell death and unnecessary systemic damage that is more common with oncological therapeutics.
- Non-invasive: With NIR light’s ability to penetrate into multiple layers of biological tissue and be absorbed by AuNRs, this technology removes the need for a light source in the body to trigger the T-cells.
- Cancer immunotherapies
- Rare disease therapies
- Autoimmune therapies
- Infectious diseases
- Tissue regeneration
Oncological immunotherapies have come a long way in the last 10 years, but many of these solutions bring their own problems, such as severe systemic toxicities and a hyper immunosuppressive environment. This results in a two-fold obstacle that the patient’s immune system must overcome in its fight against cancer: (1) the direct fight against cancer cells and (2) the harmful complications introduced by cancer treatments.
T-cells are a key component in the body’s immune response. Because of the research conducted to enhance T-cells biological killer instinct, there have been greater successes seen in patients’ response in metastatic disease. This technology takes the research a step further by allowing these formidable biological protectors to be programmed for a more precise immunotherapeutic response. The inventors envision the capabilities of non-invasive remote approach to programmable T-cells to have a broader application to various cell diseases in the future.
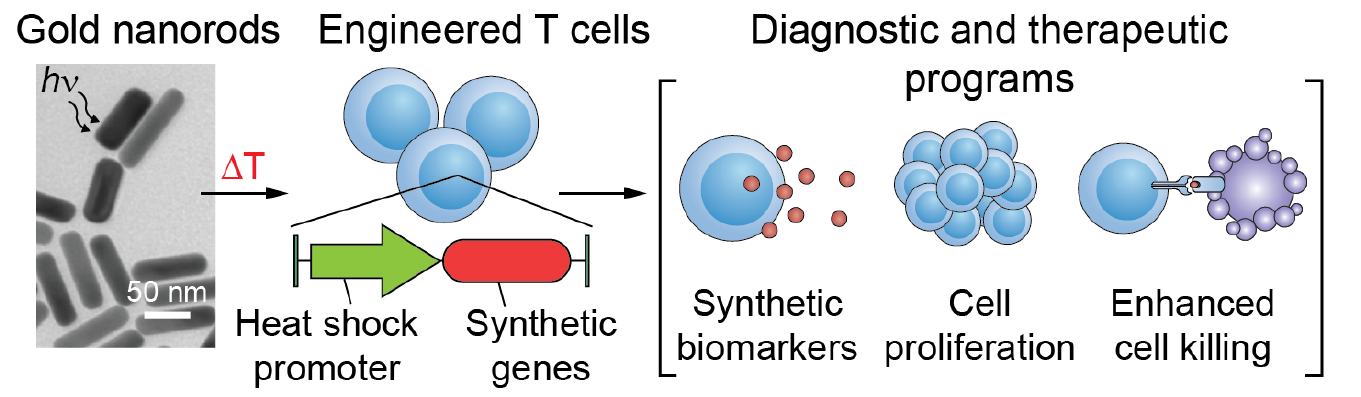
Process of photothermal genetic engineering
