Antiplatelet treatment to prevent arterial thrombi has a clinical efficacy of only about 5%
Ischemic strokes and heart attacks due to arterial blockages are responsible for nearly one in five deaths in the United States. Clots in arterial conditions are platelet-rich and formed through a mechanism known as shear-induced platelet accumulation (SIPA). These clots are resistant to treatment with anticoagulants and fibrin-directed lytic agents. During SIPA, VWF, a blood protein that helps the blood clot, is bound by platelets and rapidly releases even more VWF. This can very quickly lead to the formation of a network of platelet aggregates that can span a stenotic artery in less than an hour.
Nonetheless, the current approach to prevent thrombosis is the use of either anticoagulants to reduce thrombin-activated thrombosis or antiplatelet agents, which are the primary clinical treatment method. The clinical efficacy of antiplatelet agents to prevent thrombi is only about 5%, with an additional 5% of treated patients experiencing severe bleeding. A better treatment method is needed.
Anti-VWF agents are safer and more effective for preventing thrombotic occlusion
This technology shifts the treatment focus away from removing VWF, cleaving VWF with medical devices (e.g., ECMO or artificial heart valves), or removal with antibodies. This new approach focuses on inhibiting the release of VWF to prevent the formation of occlusive thrombi in the major arteries. By using the safe and well-established free thiol N-acetylcysteine (NAC) to prevent VWF release, this approach has demonstrated a strong and lasting ability to prevent occlusive thrombi from forming in flowing blood, both in high shear in vitro systems and in murine in vivo systems.
This anti-VWF agent has the potential to be much more effective and safer, with murine models showing 100% of arterial thrombosis being prevented from total occlusion and no severe bleeding.
- Highly effective: Has shown in human blood and mice models that low doses of NAC reduce the rate of platelet aggregation, while higher doses completely prevented platelet aggregation.
- Well established: Uses the safe, Federal Drug Administration–approved drug NAC. NAC has been widely used in humans to treat paracetamol overdose and as a mucolytic compound, and it has a well-established safety profile.
- Safer: Has shown no severe bleeding diathesis in mouse models.
Potential for use as an antithrombotic medication for patients with a high risk of forming arterial thrombi, including patients with cardiovascular disease and patients undergoing angioplasty.
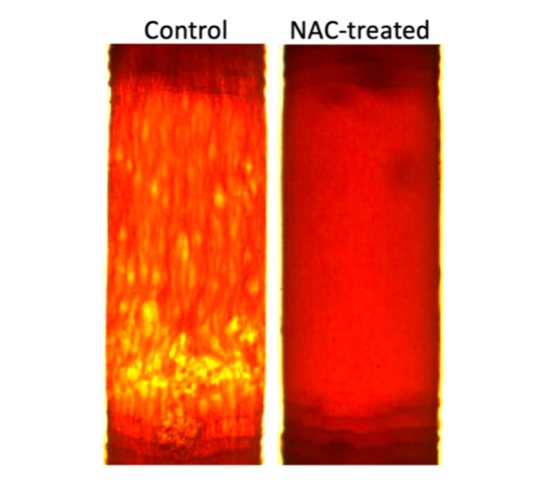
Elimination of platelet aggregation after treatment with N-acetylcysteine.
